PORTLAND, Ore. (KOIN) — Only about 8% of Oregon hospital beds are occupied by people with Coronavirus, but it is the surge in recent COVID-19 cases that have hospitals concerned they will be overwhelmed with patients on top of their normal load.
“One important note about hospital capacity is that hospitals under normal circumstances, don’t have a tremendous amount of excess capacity because that would be infrastructure and staffing we would be paying for, that we don’t need,” explained Becky Hutlberg, President and CEO of the Oregon Association of Hospitals and Health Systems.
“As we approach the winter where hospitalizations typically go up for lots of reasons, including the flu, the capacity we have will not be sufficient.”
According to the Oregon Health Authority there are 5,930 hospital beds in Oregon. 445 are occupied by patients with confirmed or suspected COVID-19. Of those patients, 102 are in intensive care units.
While those numbers are a small percentage of overall capacity, healthcare leaders say it is important to remember that not all hospital beds are created equal when it comes to a highly contagious disease.
“I think one important thing to remember about hospital beds is not all hospital beds are fit to take a COVID patient,” said Hultberg. “When you look at hospital bed counts, you’re looking at pediatric floors. You’re looking at mother-baby units. Not all those beds are available immediately for COVID patients.”
This week OHSU said it was at 89% capacity, while its four intensive care units are 93% full. Across Oregon, there are 136 adult ICU beds available out of 696.
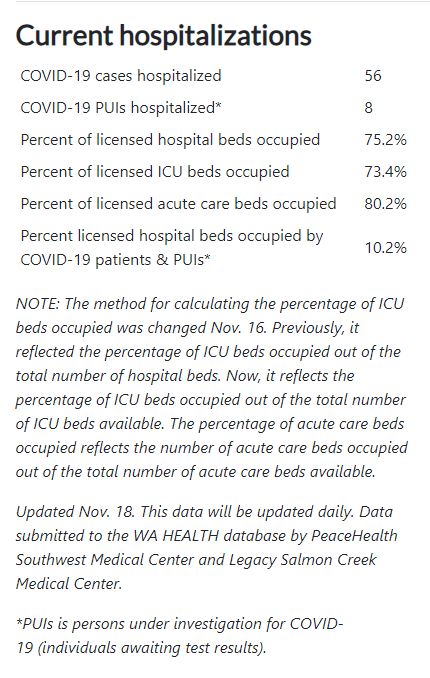
In Southwest Washington, Clark County is reporting 64 patients hospitalized with COVID-19 or who are suspected of having it. That accounts for 10% of total hospital bed capacity. Overall, 75% of hospital beds in Clark County are occupied and 73% of ICU beds are full.
Hutlberg said local hospitals have worked hard to increase bed capacity for Coronavirus patients, but a pressing problem in this latest wave is having enough staff to treat them. She said in the first two waves of the pandemic locally, hospitals could bring in staff from other regions of the country to provide relief. Now that the cases are rising nationwide, Hultberg says those supplemental workers are not available.
“And unfortunately when you see case numbers rising in the community, what you also see is caregivers getting sick in the community and then those caregivers are not available to go into work,” said Hultberg.
“It does us no good to have a hospital bed if we don’t have staff to care for the patient in that bed.”